February 2023
“Documentation burden” — you hear this phrase a lot these days, but what does it mean? It’s a term used to describe the ever-growing amount of documentation requirements placed on clinicians. It includes entering the necessary data in the EHR as well as capturing it in a format that’s usable by the many interested parties and integrations on the back end.
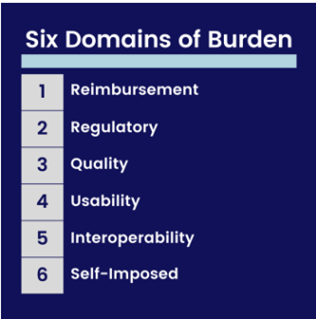
The American Nursing Informatics Association (ANIA) has developed a framework to understand the six domains that contribute to documentation burden (see the chart below).
In fact, documentation burden has become such a concern that national efforts have been made to reduce it to 25% of its current level by 2025. This goal was shared by the National Library of Medicine (NLM) through the 25 By 5 Symposium Series, sponsored by the AMIA, NLM, Columbia University Department of Medical Bioethics and Vanderbilt Medical University Center.
Great work is also taking place here at Houston Methodist to decrease documentation burden, including:
Short term efforts: Your nursing informatics and IT teams are working to streamline documentation, tasks and decision support alerts. One of our current priorities is to create a nursing shift navigator that allows for a single place to access commonly used and required documentation components for your shift. We’ve also partnered with our training team to improve your Epic training experience.
Long term efforts: The Center for Innovation and our informatics teams continue to look at ways to automate documentation. Examples include exploring ambient intelligent devices like the monitoring pilot at HMH and partnering with vendors like Epic and Nuance to create a way to capture your documentation with speech recognition.
If you have ideas on other ways we can address documentation burden, please let me know by clicking here.

Lisa Stephenson, MSN, RN-BC
Chief Nursing Informatics Officer